Introduction [1–4]
Over recent decades, human dietary patterns have shifted markedly toward increased consumption of ultra-processed foods, sugar-sweetened beverages, and refined carbohydrates. This transition has paralleled the global rise in obesity, type 2 diabetes, and metabolic disorders. Notably, recent epidemiological and experimental studies indicate that metabolic dysfunction affects not only cardiovascular and endocrine systems but is also closely linked to cognitive decline and Alzheimer’s disease. Increasing evidence characterizes Alzheimer’s disease as a disorder with a strong metabolic component in the brain, marked by neural insulin resistance, impaired glucose utilization, and disrupted cellular energy metabolism. Data from human studies, animal models, and mechanistic analyses suggest that diets high in sugar and refined carbohydrates may promote insulin resistance, mitochondrial dysfunction, neuroinflammation, and amyloid-β accumulation — all key processes in neurodegeneration.
In contrast, high-quality carbohydrates and functional polysaccharides such as glucomannan show potential to modulate postprandial glycemic responses, improve gut microbiota, and support neural energy metabolism. These findings highlight important opportunities for nutritional science and food technology in early dietary interventions aimed at reducing neurodegenerative risk.
Refined Carbohydrates and Ultra-Processed Foods in Modern Diets [2]
Refined carbohydrates are widely present in modern diets, particularly in products such as white bread, breakfast cereals, packaged snacks, sweetened beverages, processed sauces, and many frozen foods. According to the NOVA classification system, most of these carbohydrate sources fall into processed and ultra-processed food categories, typically characterized by high added sugar content but low micronutrients and dietary fiber.
During processing, much of the natural grain structure — including bran, germ, and fiber — is removed. As a result, refined carbohydrates are rapidly digested and absorbed, leading to sharp postprandial glucose spikes and strong insulin responses. When repeated frequently, this pattern reduces insulin sensitivity, promotes insulin resistance, increases visceral fat accumulation, and disrupts hunger–satiety regulation. Misleading “whole grain” labeling also contributes to confusion, as many marketed products still contain large proportions of refined flour. This increases the likelihood of consuming low-quality carbohydrates even among health-conscious consumers.
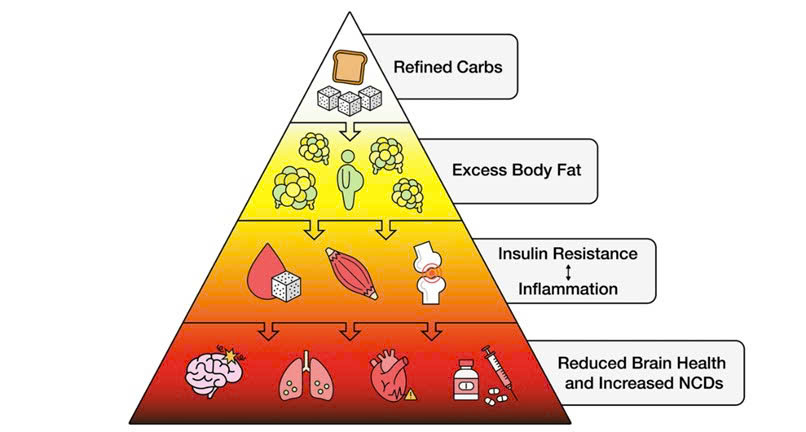
Figure 1. Mechanistic diagram linking refined carbohydrate intake with reduced brain health.
Epidemiological Evidence: Sugar Intake and Dementia Risk [3]
A community-based cohort study of older adults from the Rush Memory and Aging Project examined associations between dietary sugar intake and dementia risk using validated food frequency questionnaires and long-term clinical follow-up. Results showed that individuals in the highest sugar intake group had approximately double the dementia risk compared with those in the lowest group (HR ≈ 2.10). Risk increased progressively with the proportion of dietary energy derived from sugar. When analyzed by sugar type, fructose and sucrose showed the strongest associations with dementia risk, with hazard ratios of approximately 2.8 and 1.9, respectively, in the highest intake groups. Major sources included sugar-sweetened beverages, industrial desserts, and commercial cereals.
These findings align with evidence from MIND and Mediterranean dietary patterns, which have demonstrated neuroprotective effects and emphasize limiting sugary and ultra-processed foods.
Mechanisms Linking High-Sugar Diets with Metabolic and Neurodegenerative Disorders [4]
Experimental studies frequently use the cafeteria diet model — high in saturated fat, refined sugar, and energy-dense foods — to simulate Western dietary patterns. Evidence shows that this model induces obesity, dyslipidemia, and insulin resistance, while also producing adverse changes in the central nervous system. Experimental animals exhibit impaired learning and memory, increased amyloid-β deposition, enhanced tau phosphorylation, neuroinflammation, and oxidative stress in brain tissue. These alterations resemble key biological features of Alzheimer’s disease and support the hypothesis that diet can directly influence neurodegenerative processes through metabolic mechanisms, not solely vascular pathways.
Mechanistically, multiple biological axes connect high sugar intake with neurodegeneration. The brain depends heavily on glucose for energy, but under insulin-resistant conditions, impaired insulin signaling reduces neuronal glucose uptake and utilization, leading to energy deficits and reduced synaptic plasticity. Chronic hyperinsulinemia also reduces amyloid-β clearance due to competition for insulin-degrading enzymes, thereby promoting amyloid accumulation. Elevated glucose and lipid levels increase reactive oxygen species production and mitochondrial dysfunction — a consistent feature in Alzheimer’s pathology. Obesity and insulin resistance further stimulate pro-inflammatory cytokine release and weaken the blood–brain barrier, allowing peripheral inflammatory signals to amplify neuroinflammation.
In addition, the gut–brain axis has emerged as an important regulatory pathway. Gut microbiota ferment dietary fiber to produce short-chain fatty acids (SCFAs), which strengthen gut barrier integrity, modulate immunity, and support neural energy metabolism. In animal models, SCFAs are also associated with reduced amyloid deposition and tau pathology.
Beneficial Carbohydrates and Brain-Protective Diets: Food-Based Interventions [3,4]
From a food science and technology perspective, functional polysaccharides such as glucomannan can form gels and increase digestive viscosity, thereby slowing glucose absorption, lowering postprandial glycemic peaks, and reducing insulin demand. They also support gut microbiota and weight control. Thus, developing foods rich in functional fibers and slow-digesting structures represents an important direction in functional and medical nutrition. Mediterranean and MIND dietary patterns — rich in plant foods and fiber while limiting added sugars — are associated with reduced risks of cognitive decline and Alzheimer’s disease, highlighting the preventive potential of carbohydrate quality–focused dietary strategies.
Conclusion [1–4]
Current epidemiological, experimental, and mechanistic evidence indicates that diets high in sugar and refined carbohydrates contribute significantly to metabolic dysfunction and increased neurodegenerative risk. Key mechanisms include insulin resistance, oxidative stress, neuroinflammation, mitochondrial impairment, and amyloid accumulation. Conversely, high-quality carbohydrates and functional polysaccharides may exert protective effects through glycemic regulation and gut microbiota modulation.
For biological and food technology fields, these findings support the development of novel food systems enriched with functional fiber and controlled-absorption carbohydrates to help prevent metabolic disease and promote long-term brain health.
References:
- Lee, E., Hwang, J., Kim, D. W., Choi, B. Y., Bae, H. J., Won, S. H., ... & Kim, S. (2026). Association between high carbohydrate to dietary fiber ratio and risk of dementia in older adults: analysis from the UK biobank. BMC neurology, 26(1), 33.
- Maffetone, P., & Laursen, P. B. (2025). Refined carbohydrates and the overfat pandemic: implications for brain health and public health policy. Frontiers in Public Health, 13, 1585680.
- Agarwal, P., Ford, C. N., Leurgans, S. E., Beck, T., Desai, P., Dhana, K., ... & Bennett, D. A. (2023). Dietary sugar intake associated with a higher risk of dementia in community-dwelling older adults. Journal of Alzheimer’s Disease, 95(4), 1417-1425.
- Abubakar, M., Giri, A., Goel, F., Khan, M., Gupta, J., Kumar, D., ... & Kumar, N. (2025). Diabetes, Alzheimer's disease risk factors, and the cafeteria diet: a comprehensive review. Current neuropharmacology.